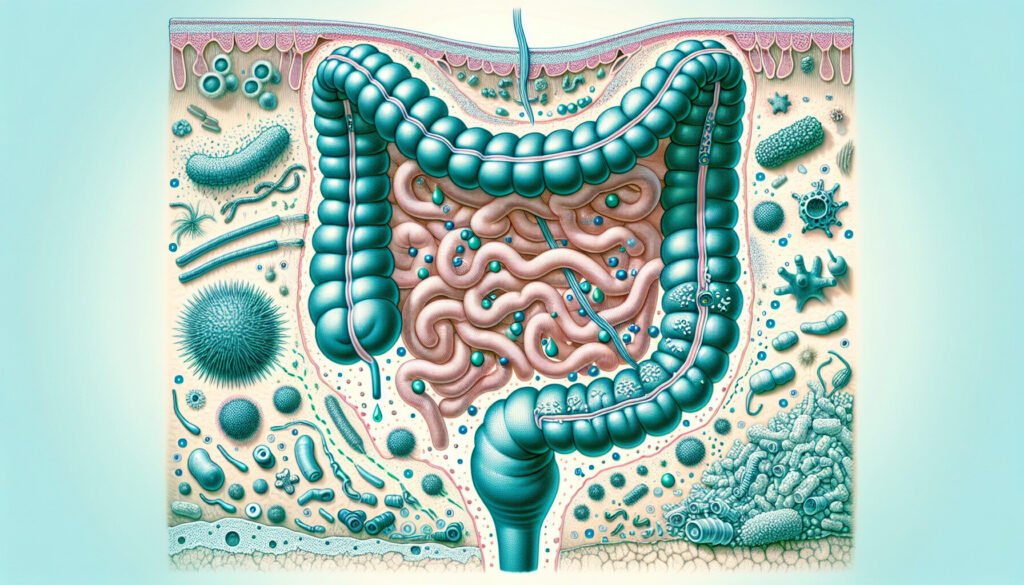
The link between gut microbiota and alcohol use disorder has been a topic of interest for researchers at Tufts University School of Medicine and Tufts Graduate School of Biomedical Sciences. In a recent study published in the journal mBio, scientists have uncovered a surprising connection between a fungus commonly found in the human gut, Candida albicans, and the brain’s dopamine reward pathway.
The research conducted in mice revealed that an overgrowth of C. albicans led to an increase in inflammatory molecules known as PGE2. These molecules have the ability to cross the blood-brain barrier and impact the desire for alcohol. As C. albicans thrives in the gut due to factors like antibiotic use, poor diet, or alcohol consumption, it triggers the production of PGE2. The study suggests that as these molecules travel to the forebrain, they alter dopamine signaling in the dorsal striatum, a region crucial for reward processing and habit formation.
Contrary to the researchers’ initial hypothesis that mice colonized with C. albicans would find alcohol more rewarding, the study results showed the opposite. As PGE2 levels rose alongside fungal populations, the mice actually avoided consuming alcohol. However, when the researchers blocked the PGE2 receptor molecules, the mice resumed drinking alcohol.
Lead author Andrew Day noted, “Our study shows how science works—our initial ideas were very wrong. This could be explained by differences in how mice respond to C. albicans compared to humans, differences in fungal strains, or we might be seeing a small snapshot of the entire story.”
Additionally, the researchers observed that mice with C. albicans overgrowth were more sensitive to alcohol’s effects on motor coordination. This effect could also be reversed by blocking PGE2 activity.
Senior author Carol Kumamoto emphasized the significance of fungi in the gut-brain axis, stating, “Our bodies are wired so that our behavior responds to gut microbiota, and this study highlights that fungi are important components of the gut-brain axis.”
Alcohol use disorder affects a significant portion of the global population, with traditional treatments showing moderate effectiveness. The findings of this study may pave the way for new approaches to understanding and addressing alcohol use disorder. Future investigations into the role of fungi and PGE2 in this condition could unveil novel contributors to its progression.
In conclusion, the study sheds light on the complex interplay between gut microbiota, fungal colonization, and alcohol consumption. By unraveling the mechanisms through which C. albicans and PGE2 influence the brain’s reward system, researchers hope to develop innovative strategies for managing alcohol use disorder. Stay tuned for further developments in this exciting field of research.