A groundbreaking study conducted by researchers at Columbia University Mailman School of Public Health, Columbia University Irving Medical Center, and the Butler Columbia Aging Center has revealed a new perspective on the metabolic hormone FGF21. Published in Nature Metabolism, the study demonstrates how FGF21 not only plays a role in metabolism, glucose regulation, and diabetes but also acts as a stress hormone, connecting psychological stress to metabolic dysregulation and physical disease.
For over two decades, FGF21 has been a subject of research for its metabolic functions. However, this study is the first to show how psychological stress can acutely alter FGF21 levels in the bloodstream. This discovery sheds light on how mental states can impact metabolic responses, influencing overall health and biological aging.
Senior author Martin Picard, Ph.D., associate professor of behavioral medicine at Columbia, emphasized the significance of this finding, stating that FGF21 acts as a “hormonal bridge between body and mind,” integrating psychosocial experiences with systemic metabolic signaling beyond traditional stress hormones.
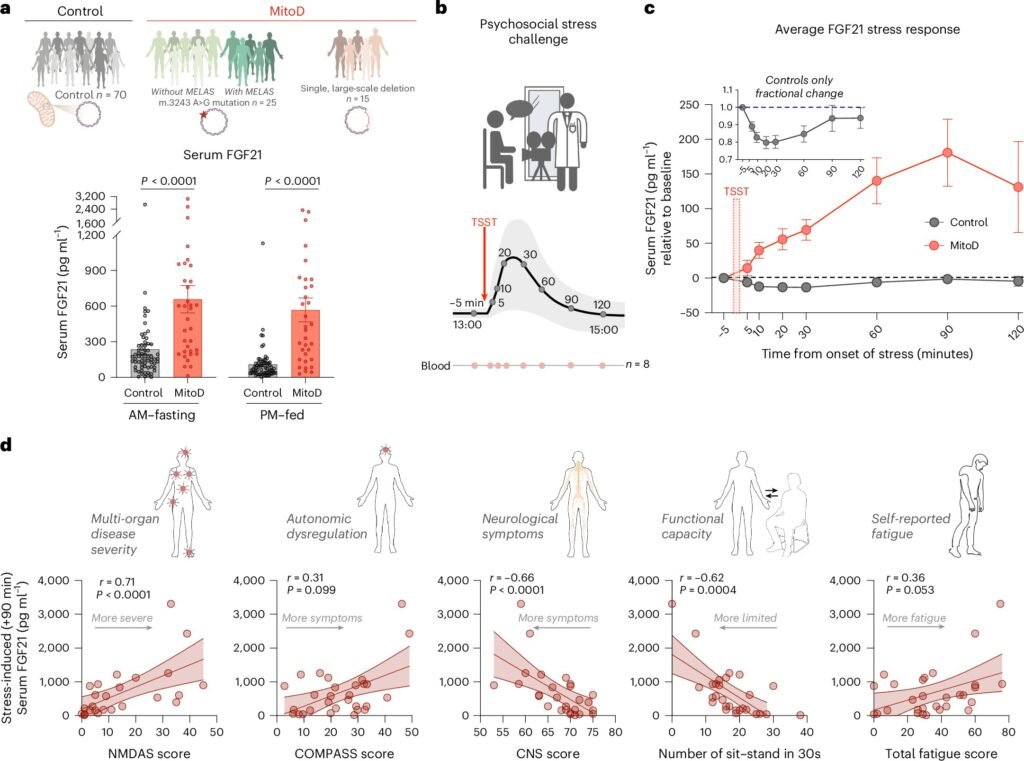
The study observed hormonal changes following acute psychological stress in both healthy individuals and patients with mitochondrial disease, a group of genetic disorders affecting cellular energy transformation. In healthy participants, FGF21 levels initially dropped after exposure to stress, returning to baseline within 90 minutes. On the other hand, participants with impaired mitochondrial function showed an increase in FGF21 levels following stress, indicating a distinct stress response influenced by mitochondrial biology.
Lead author Mangesh Kurade highlighted the implications of these results, noting that social and psychological environments can directly impact metabolic outcomes and disease risk. The study’s population-level analysis revealed that factors like loneliness, childhood neglect, and relationship breakdowns were associated with higher FGF21 levels, while positive social interactions and emotional well-being correlated with lower levels.
The validation of these findings through large-scale data analysis and the ongoing MiSBIE study further strengthens the role of FGF21 as a reliable biomarker for understanding how psychosocial factors influence metabolic biology and clinical outcomes in mitochondrial diseases.
By identifying FGF21 as a mediator and biomarker of psychological stress, the study opens up new avenues for research and clinical monitoring. The integration of FGF21 and other biomarkers into precision mental health strategies could enhance the assessment of metabolic stress vulnerability and therapeutic responses.
In conclusion, FGF21’s dual role as a metabolic hormone and stress mediator underscores its significance in bridging the gap between mind and body. This study marks a pivotal moment in understanding how our experiences, relationships, and resilience are translated into biological responses. As we continue to unravel the complexities of human health, the exploration of FGF21 offers promising insights into the aging process, adaptation, and response to stress.