Climate change and failing to meet sustainable development goals could lead to a surge in antimicrobial resistance (AMR) by 2050, as per a recent study published in Nature Medicine. The research projects a potential global increase of up to 2.4% in AMR by 2050, highlighting the need for immediate action to address broader socioeconomic and environmental factors beyond just reducing antibiotic usage to combat the growing AMR crisis.
In 2021, bacterial AMR was responsible for around 1.14 million deaths worldwide, with a disproportionate impact on low- and middle-income countries. This figure is projected to rise to nearly 2 million deaths by 2050. To tackle this alarming trend, global leaders at the 79th United Nations General Assembly committed to reducing the estimated 4.95 million annual deaths related to bacterial AMR by 10% by 2030.
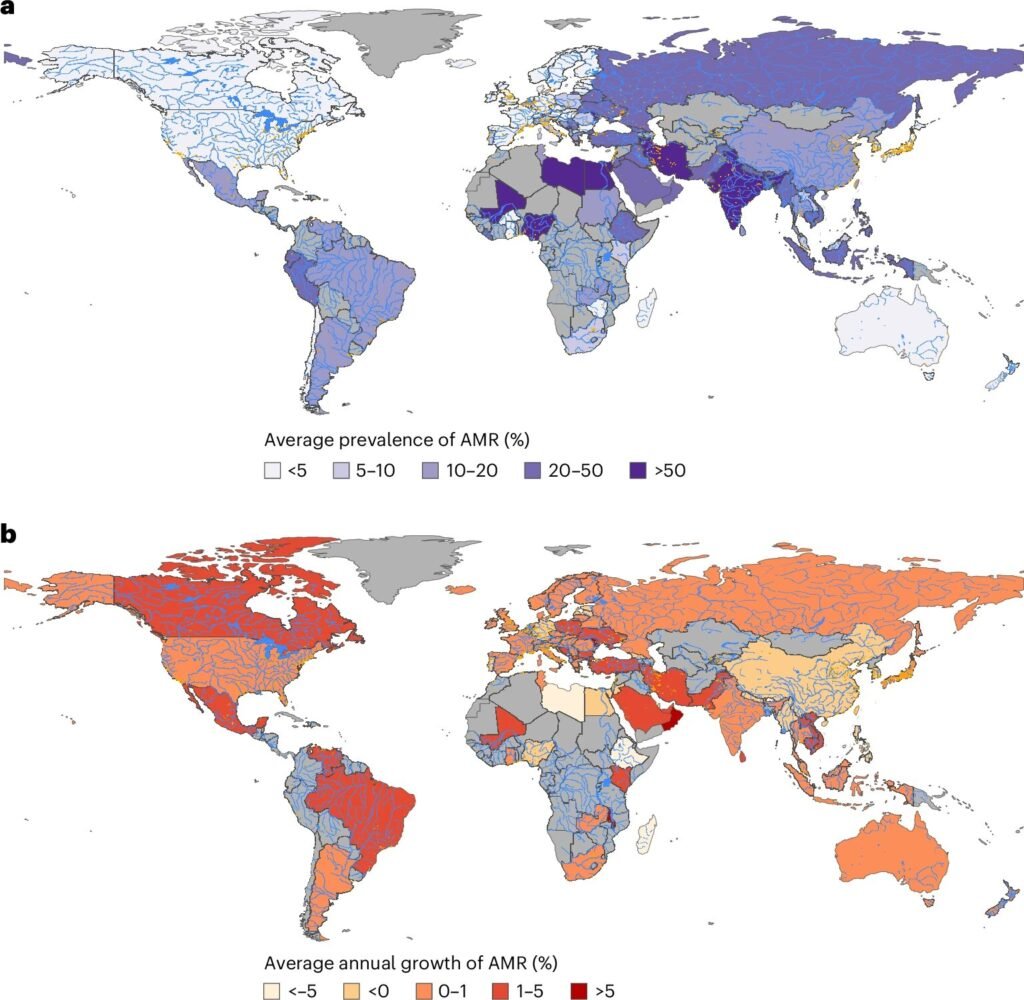
While efforts to combat AMR have primarily focused on curbing antibiotic overuse, the study emphasizes the importance of considering the implications of climate change and socioeconomic conditions. Research conducted by Lianping Yang and his team involved analyzing data from 4,502 records comprising 32 million isolates of six key bacterial pathogens resistant to antimicrobials across 101 countries from 1999 to 2022. By employing forecasting models, they assessed how socioeconomic and environmental factors, alongside policies, could impact global AMR trends.
Under a worst-case scenario of climate change adaptation, where global temperatures could surge by 4–5°C by the end of the century, AMR could escalate by 2.4% by 2050 compared to a low-emission scenario. This increase varied between 0.9% in high-income nations and 4.1% and 3.3% in lower-middle-income and lower-income countries, respectively.
The study also highlighted that sustainable development initiatives, such as reducing out-of-pocket health expenses, expanding immunization coverage, boosting health investments, and ensuring universal access to water, sanitation, and hygiene services, could potentially lower the prevalence of AMR by 5.1% compared to baseline projections. This impact surpasses the effect of reducing antimicrobial consumption, which is estimated to decrease AMR prevalence by 2.1%.
While the research sheds light on the critical intersection of climate change, socioeconomic factors, and AMR, the authors caution that the study’s ecological modeling approach limits the ability to establish causality. Additionally, certain factors contributing to AMR, such as education levels, antimicrobial use in food production, and animal farming practices, were not fully considered due to data limitations.
For more insights, refer to the study titled “Changing climate and socioeconomic factors contribute to global antimicrobial resistance” published in Nature Medicine. (DOI: 10.1038/s41591-025-03629-3)
As the world grapples with the escalating threat of antimicrobial resistance, it is imperative to adopt a comprehensive approach that addresses the complex interplay of environmental, economic, and societal factors to safeguard public health and combat this global health crisis.