A groundbreaking study published in Nature has uncovered a surprising side effect of high-dose radiation therapy on metastatic tumors. Researchers at the University of Chicago Medicine Comprehensive Cancer Center have identified a phenomenon where radiation can actually cause growth in existing metastatic tumors that were not directly treated with radiation.
This unexpected response has been named the “badscopal effect” by the researchers, as it is the opposite of the well-known “abscopal effect” where radiation causes distant tumors to shrink. The study found that high doses of radiation can increase the production of a protein called amphiregulin by tumor cells that are directly treated with radiation. This protein weakens the immune system’s ability to fight cancer and enhances the ability of cancer cells to protect themselves.
Radiotherapy, which is commonly used to control localized tumors, has been shown to have a dual effect when it comes to metastatic tumors. While it can activate the immune system and lead to regression in distant tumors (abscopal effect), it can also promote growth in existing metastases (badscopal effect). This new understanding of the interaction between radiation and metastatic tumors opens up promising new therapeutic strategies for more effective treatments in metastatic cancer cases.
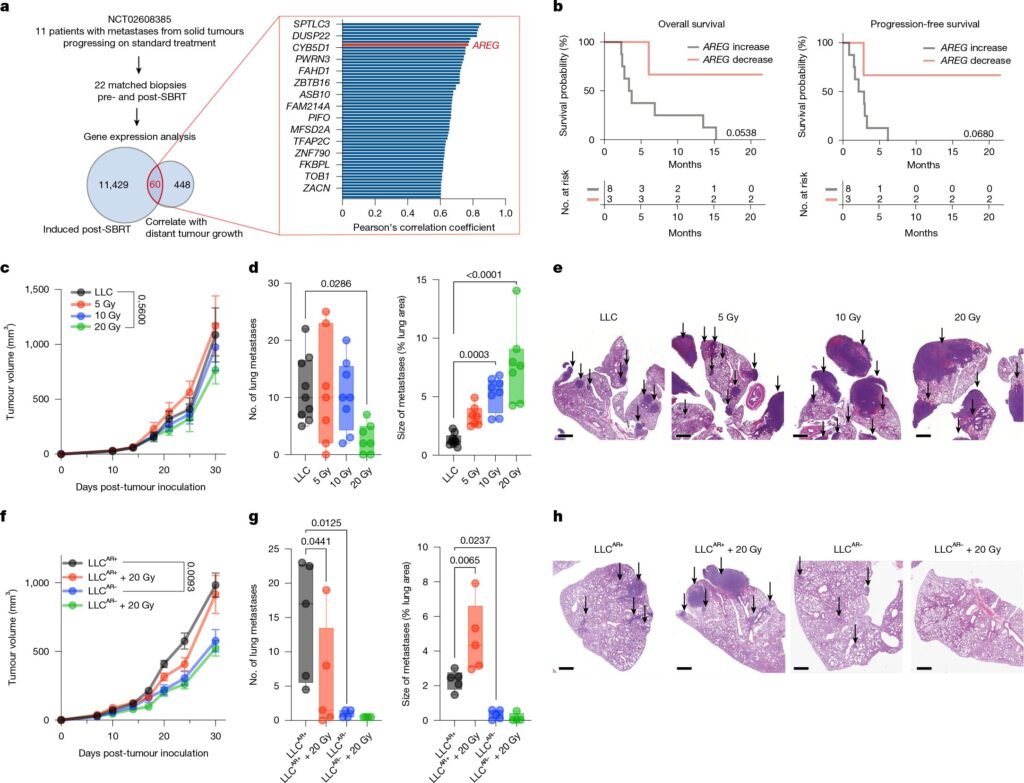
The research team, led by senior author Ralph Weichselbaum, MD, conducted gene expression profiling of patient tumors before and after radiation treatment to uncover the mechanism behind the badscopal effect. They discovered that amphiregulin levels were significantly increased in tumors that had been treated with radiation, leading to enhanced growth in existing metastatic sites.
Further studies using animal models of lung and breast cancer confirmed the role of amphiregulin in promoting tumor growth after radiation. By blocking amphiregulin with antibodies or genetic editing techniques, the researchers were able to reduce the size of tumors outside of the radiation field. Combining radiation with amphiregulin blockade showed significant improvements in controlling metastatic tumors.
The study also explored the role of immune suppression in the badscopal effect. Analysis of blood samples from lung cancer patients receiving radiation and immunotherapy revealed that high levels of amphiregulin were associated with adverse outcomes. Additionally, an increase in immunosuppressive myeloid cells was linked to metastasis progression and death.
By targeting molecules like amphiregulin and CD47, which are upregulated by radiation, in combination with radiotherapy, the researchers were able to achieve effective metastatic control in animal models. This paradigm shift in the use of radiation therapy could lead to personalized treatments for patients with metastatic disease.
The results of this study pave the way for future clinical trials to validate these findings and explore new treatment strategies for metastatic cancer patients. The potential for personalized radiotherapy based on the systemic effects of radiation offers hope for more effective and targeted cancer treatments in the future.