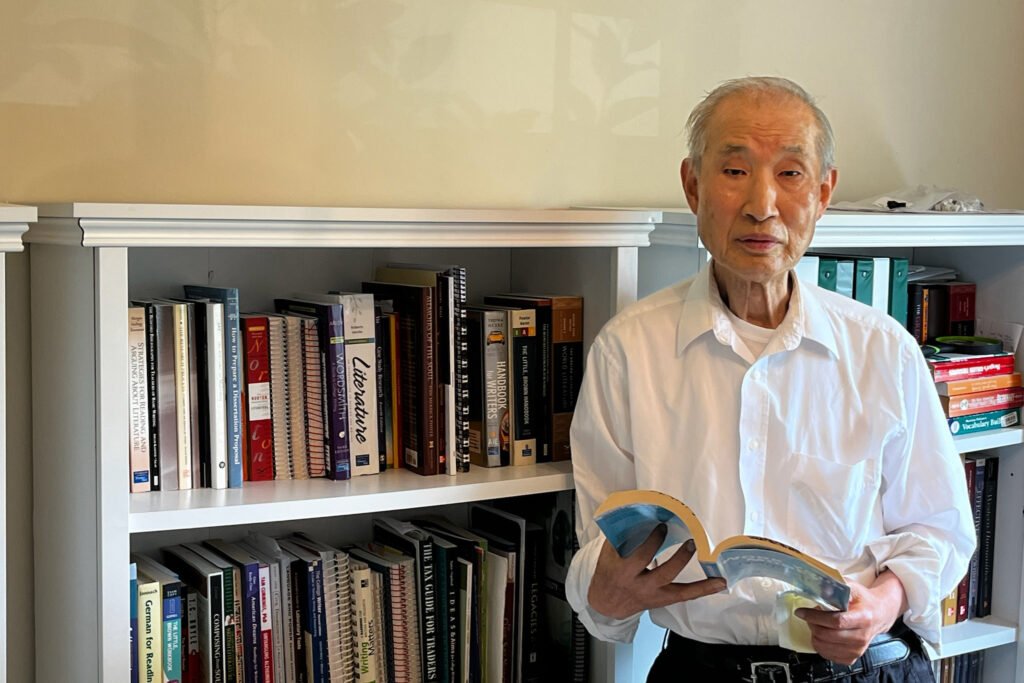
Chikao Tsubaki, an octogenarian, had been facing a series of health challenges in his mid-80s. First, a stroke, then lymphoma, followed by prostate cancer. These ailments left him fatigued, isolated, and unsteady on his feet. However, his life took a positive turn when he participated in an innovative care initiative known as Community Aging in Place: Advancing Better Living for Elders (CAPABLE).
Over a span of four months, a team comprising an occupational therapist, a nurse, and a handy worker visited Tsubaki’s home to assess his needs and ensure his safety. Along with installing grab bars and rails, the handy worker even built a bookshelf to prevent Tsubaki or his beloved books from toppling over. Reading was Tsubaki’s way of exercising his brain, and he credits it for his cognitive health. Now 87 years old, he lives independently and walks almost one and a half miles every day.
Despite its proven effectiveness, CAPABLE remains relatively small, having served around 4,600 individuals to date. One of the major obstacles to its wider implementation is the lack of insurance coverage. Traditional Medicare and most Medicare Advantage plans do not cover the program, leaving it reliant on grants from state agencies and philanthropic organizations for funding.
The payment challenges faced by CAPABLE highlight a broader issue in the healthcare system, where funding is primarily directed towards treating existing illnesses rather than preventive community services. Medicare lacks billing codes for interventions aimed at preventing health issues, making it difficult for programs like CAPABLE to secure reimbursement.
Sarah Szanton, the co-creator of CAPABLE, developed the program based on her experiences as a nurse practitioner making home visits in Baltimore. Inspired by the success of a similar program called ABLE, Szanton expanded the model to include a nurse for medication management and mental well-being checks. CAPABLE operates on a participatory approach, with clients and the care team collaborating to address individual needs.
While CAPABLE may not be a one-size-fits-all solution for all older adults, studies have shown that it significantly improves safety and mobility for participants. Additionally, it has the potential to generate Medicare savings of approximately $20,000 per person over a two-year period post-intervention.
As the healthcare landscape evolves, there is growing interest in expanding coverage for innovative programs like CAPABLE. With the right parameters and safeguards in place, Medicare could potentially include such preventive services as part of its coverage. For individuals like Tsubaki, who have benefited greatly from the program, the impact of CAPABLE on their independence and quality of life is undeniable.