Organoid technology has taken a major step forward with the recent breakthrough achieved by scientists from Cincinnati Children’s and their colleagues in Japan. They have successfully produced liver tissue that is capable of growing its own internal blood vessels, a development that holds great promise for individuals living with hemophilia and other coagulation disorders. Additionally, this advancement brings us closer to the possibility of creating transplantable repair tissues for individuals with damaged livers.
The study, led by Dr. Takanori Takebe, was recently published in Nature Biomedical Engineering. Collaborating with researchers from the Institute of Science Tokyo, the Icahn School of Medicine at Mount Sinai, and Takeda Pharmaceutical Company, the team has made significant progress in understanding and replicating the complex cellular interactions involved in liver development.
Organoids are lab-grown human organ tissues that have become invaluable tools for medical research. By placing induced pluripotent stem cells (iPSCs) in special gels designed to promote specific tissue growth, researchers can mimic the development of organ-specific structures. Cincinnati Children’s has been at the forefront of organoid research since 2010 when they successfully developed the first functional intestinal organoid from iPSCs.
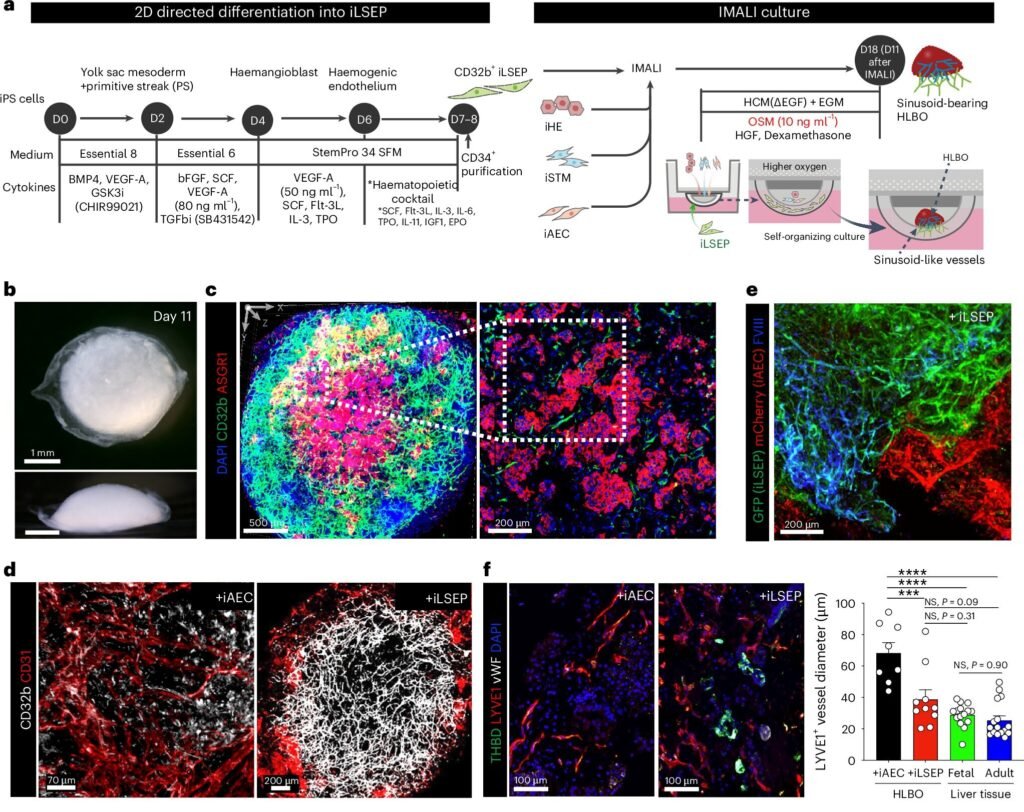
One of the challenges in growing organoids has been the limitation in size due to the absence of essential tissues like nerves and blood vessels. However, the recent study successfully overcame this obstacle by differentiating human pluripotent stem cells into liver sinusoidal endothelial progenitors (iLSEP). Using an innovative culture system, the team supported the self-organization of these progenitor cells into hepatic endoderm, septum mesenchyme, arterial, and sinusoidal quadruple progenitors.
The advanced organoids produced functional blood vessels with sinusoid-like features, capable of producing essential blood coagulation factors. In mice with hemophilia, the organoid-derived Factor VIII was able to rescue them from severe bleeding, showcasing the potential of this technology in treating coagulation disorders.
With an estimated 33,000 males in the U.S. living with hemophilia, this breakthrough could revolutionize treatment options for these individuals. By producing coagulation factors and potentially serving as a source for repair tissues, these advanced liver organoids offer hope for improved outcomes in hemophilia and liver failure cases.
In conclusion, the development of organ-specific blood vessels in liver organoids represents a significant advancement in the field of regenerative medicine. With further research and refinement, this technology could pave the way for personalized treatments and improved outcomes for individuals with a range of medical conditions.