He decided to take matters into his own hands and seek out a more cost-effective solution. After researching different options, he discovered a pharmacy benefit manager (PBM) that could offer significant savings on prescription medications for his staff members.
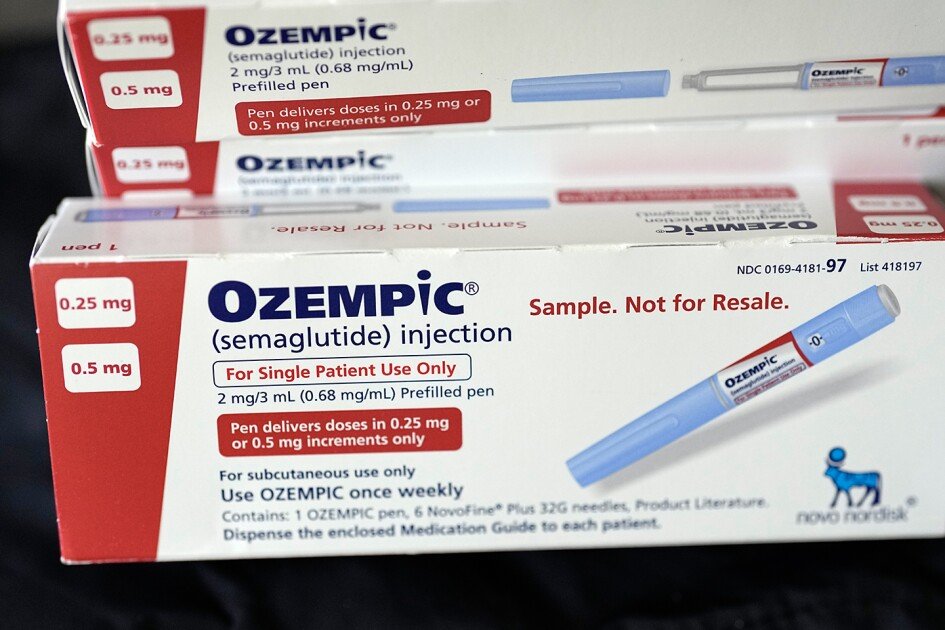
By partnering with this PBM, the districts under the Pikes Peak Board of Educational Services were able to negotiate lower prices on medications like Ozempic and other expensive drugs. This not only helped to alleviate the financial burden on staff members but also allowed the districts to maintain their health insurance coverage without sacrificing other essential programs and services.
Bershinsky’s proactive approach to addressing rising health-care costs serves as a model for other school districts struggling to navigate the challenges posed by expensive prescription medications. By exploring alternative options and advocating for more affordable pricing from pharmaceutical companies, districts can ensure that their employees have access to the medications they need without breaking the budget.
As policymakers and lawmakers continue to grapple with the issue of rising health-care costs, it is crucial for school districts to be proactive in finding solutions that work for their staff members. The case of Casey Jakubowski and the challenges he faces in accessing Ozempic serves as a stark reminder of the impact that expensive medications can have on individuals and organizations alike.
In the face of these challenges, it is essential for school districts to prioritize the health and well-being of their staff members while also being mindful of their financial resources. By working together to find creative solutions and advocate for more affordable options, districts can ensure that their employees receive the care they need without sacrificing other essential programs and services. Colorado Springs school district superintendent, Michael Bershinsky, took a bold step in addressing the healthcare needs of his staff by pursuing a partially self-funded health insurance arrangement. This new approach aims to provide a more tailored and cost-effective solution that caters to the individual needs of participating employees.
The district’s new insurance provider has partnered with a company that sources expensive prescription medications such as Ozempic and Humera from countries like Australia and Canada. Under this arrangement, the district pays a flat fee of $3,000 per staff member per year, and staff members incur no out-of-pocket costs for these medications. This innovative approach not only ensures access to vital medications but also helps in controlling healthcare costs for the district.
According to a survey conducted by the EdWeek Research Center, slightly more than half of district leaders rely on national companies as their primary health insurance providers. However, Bershinsky’s decision to move away from major firms highlights the potential benefits of exploring alternative options. While this approach may not be suitable for every district, it underscores the importance of strategic planning and collaboration among administrators to find the best healthcare solutions for their staff.
Bershinsky emphasizes that implementing a new healthcare arrangement requires time, effort, and the support of various stakeholders. It is not as simple as renewing the existing insurance contract but involves careful consideration of the unique needs and preferences of the staff. By thinking outside the box and exploring innovative solutions, districts can potentially improve healthcare outcomes for their employees while managing costs effectively.
In conclusion, Bershinsky’s proactive approach to healthcare management serves as a testament to the importance of exploring alternative solutions to meet the evolving needs of staff. By embracing a partially self-funded model and collaborating with innovative partners, districts can create a more personalized and cost-effective healthcare system that prioritizes the well-being of their employees.