“PBMs continue to operate in the shadows, driving up costs for patients and making it harder for them to access the medicines they need. We urge Congress to prioritize PBM reform in the upcoming legislative session to ensure patients have access to affordable medications.”
State-level action
While federal PBM reform efforts have stalled, several states have taken matters into their own hands to regulate PBMs. California, for example, passed a landmark bill in October that prohibits PBMs from charging patients more for a drug than the pharmacy’s acquisition cost, among other provisions. The law also requires PBMs to disclose rebate amounts to health plans and how much they are keeping for themselves.
Similar laws have been passed in Arkansas, Connecticut, and Georgia, and more states are expected to follow suit in 2025. These state-level actions may pave the way for federal reform by demonstrating the impact of PBM regulation on drug prices and patient access.
The road ahead
As the healthcare landscape continues to evolve, PBMs are under increasing pressure to reform their business practices and increase transparency. With the FTC’s lawsuit against the Big Three PBMs and state-level actions gaining momentum, 2025 could be a pivotal year for PBM reform.
Pharma companies, lawmakers, and patient advocacy groups are all pushing for change to rein in drug costs and ensure fair competition in the pharmaceutical market. Whether these efforts will succeed remains to be seen, but one thing is clear: the status quo of PBMs in the healthcare industry is no longer sustainable.
Stay tuned as the battle for PBM reform unfolds in the coming months, shaping the future of drug pricing and access for millions of patients across the country.
In recent years, pharmacy benefit managers (PBMs) have come under increasing scrutiny for their role in driving up drug costs in the healthcare industry. As middlemen between health insurers, pharmacies, and patients, PBMs negotiate drug prices and design formulary plans, claiming to mediate cost efficiency for their clients. However, critics argue that the PBM rebate system is opaque and leads to inflated drug costs, while their joint ownership structure with pharmacies and health insurers creates an unfair and anticompetitive business model.
The three major PBM companies – CVS’s Caremark, Cigna’s Express Scripts, and UnitedHealthcare’s OptumRx – control a significant portion of the market, leading to concerns about their concentrated and complex operations. Calls for PBM reform have been growing louder, with lawmakers, the pharma industry, and health insurers all pushing for change.
The Federal Trade Commission (FTC) took a significant step in July last year by publishing a report that blamed PBMs for higher drug prices. In September, the agency sued the major PBMs for artificially inflating the price of insulin and engaging in anticompetitive behavior. This lawsuit marked a turning point in the fight against PBMs and their practices.
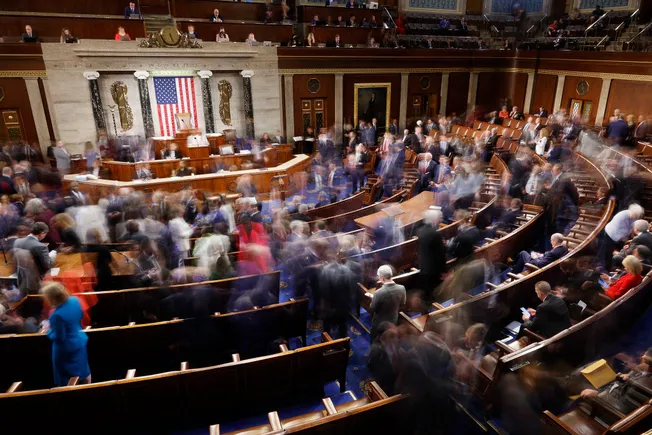
Legislative efforts to reform PBMs have faced challenges in Congress, with various bills failing to gain traction. A recent federal funding bill included provisions for PBM reform, but the bill was ultimately stripped down before passing. Despite these setbacks, industry groups and lawmakers continue to push for PBM reform at the federal level.
While federal efforts have stalled, several states have taken action to regulate PBMs. California passed a landmark bill in October that imposes restrictions on PBM practices and increases transparency requirements. Other states are expected to follow suit in 2025, potentially paving the way for broader federal reform.
As the pressure mounts on PBMs to reform their practices and increase transparency, 2025 could be a pivotal year for PBM reform. With ongoing lawsuits, state-level actions, and continued advocacy for change, the future of PBMs in the healthcare industry remains uncertain. Patients, lawmakers, and industry stakeholders are all closely watching as the battle for PBM reform unfolds in the coming months, with the goal of ensuring fair competition and affordable drug access for all. The healthcare system in the United States has long been plagued by issues related to pharmacy benefit managers (PBMs). These entities, which act as middlemen between drug manufacturers, pharmacies, and insurers, have been criticized for their lack of transparency and for driving up prescription drug costs.
In response to these concerns, there has been a push for PBM reform across Congress. Senators Elizabeth Warren and Josh Hawley recently introduced The PBM Act, which aims to address some of the key issues surrounding PBMs. The bill would prohibit joint ownership of PBMs and pharmacies, as well as insurers owning pharmacy businesses. This move is seen as a way to break up the monopolies held by the top three largest PBMs, which are owned by major pharmacy chains and health insurers.
While several other bills related to PBM reform have been introduced in the past, none have been approved. The Lower Costs, More Transparency Act, which passed in the House but died in the Senate, is one example of the challenges faced in enacting meaningful reform. However, there is hope that these bills could be revisited in the new Congress.
Former President Donald Trump has also weighed in on the issue of PBMs, criticizing them as unnecessary middlemen that drive up drug costs. While his comments have led to fluctuations in the share prices of major healthcare companies, it remains to be seen if he will take concrete action on PBM reform during his second term.
Overall, the push for PBM reform has gained momentum in recent years, with bipartisan support and a growing awareness of the need for change. By working together with patients, pharmacists, providers, employers, and other stakeholders, there is hope that important reforms can be implemented to create a more transparent and cost-effective healthcare system.