Researchers from the University of Sydney have made a groundbreaking discovery in the field of pain relief. Using placebo treatments, they have uncovered a map-like system in the brainstem that controls pain in a highly specific manner depending on the location in the body where it is felt. This exciting finding could revolutionize the way chronic pain is treated, offering safer and more targeted alternatives to opioid medications.
The brainstem, often likened to a highway connecting the brain to the spinal cord, plays a crucial role in managing all signals related to pain and other bodily functions. It is responsible for producing and releasing various neurochemicals essential for cognitive processes, survival instincts, and sensory perception.
Published in the prestigious journal Science, the study utilized state-of-the-art 7-Tesla functional magnetic resonance imaging (fMRI) technology to identify how two key regions in the brainstem regulate pain through the placebo effect. Dr. Lewis Crawford, the lead author of the study and a research fellow at the School of Medical Sciences and the Brain and Mind Center, described the findings as groundbreaking. He explained that this is the first time such a detailed pain map has been observed in the human brainstem, demonstrating its ability to tailor pain relief to specific regions of the body.
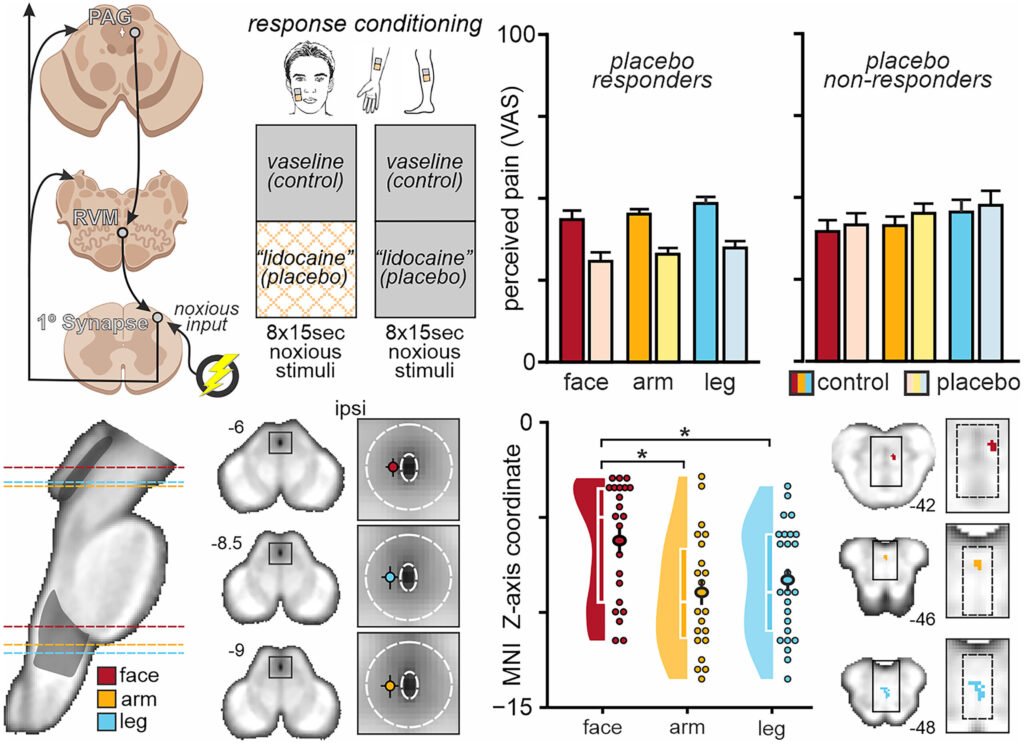
The research involved 93 healthy participants who were exposed to heat-induced pain on different body parts and treated with a placebo pain-relief cream. Surprisingly, even after the cream was removed and the pain stimulus reapplied, up to 61% of participants reported reduced pain in the area where the placebo treatment had been administered. This demonstrated a true placebo response, indicating the brain’s ability to modulate pain perception based on specific body regions.
The study identified two critical brainstem regions—the periaqueductal gray (PAG) and the rostral ventromedial medulla (RVM)—that exhibited distinct patterns of activity depending on the location of the pain relief. Upper parts of the PAG and RVM were more active in alleviating facial pain, while lower regions showed increased activity for arm or leg pain. This spatially organized pain control mechanism highlights the brain’s sophisticated ability to target pain relief to specific areas.
The implications of this research are profound, offering new possibilities for developing personalized and non-invasive pain therapies with minimal side effects. Professor Luke Henderson, the senior author of the study and a Professor in the School of Medical Sciences and the Brain and Mind Center, emphasized the potential for designing more effective treatments for chronic pain tailored to individual needs.
Moreover, the study challenges traditional beliefs about placebo pain relief mechanisms, suggesting that a distinct part of the brainstem—the lateral PAG—plays a significant role without relying on opioids. Instead, cannabinoid activity may be involved in localized pain control, presenting a novel avenue for pain management research.
By understanding how different brainstem areas are linked to specific body regions, researchers hope to develop precise treatments for chronic pain that do not depend on opioids. This groundbreaking research marks a significant advancement in the field of pain relief, offering hope for more effective and targeted therapies in the future.