A recent study conducted at Avicenna University Hospital (Cadi Ayyad University) has shed light on the potential of the plethysmographic perfusion index (PPI) as a valuable tool in identifying fluid responsiveness in critically ill patients with acute circulatory failure. Published in the Journal of Intensive Medicine, this research offers insights into a noninvasive parameter derived from pulse oximetry that could revolutionize fluid therapy management in emergency care settings.
In cases where patients experience shock or acute circulatory failure, the decision to administer intravenous fluids is crucial. Underadministration can lead to organ underperfusion, while overadministration may result in pulmonary complications like edema. While advanced hemodynamic monitors and echocardiography are typically used to guide these decisions, they may not always be readily available, especially in fast-paced emergency situations or resource-limited environments.
The PPI, a simple index generated by modern pulse oximeters, reflects the ratio of pulsatile to nonpulsatile blood flow detected in the fingertip or earlobe. Changes in PPI following a fluid bolus could potentially mirror changes in cardiac output, making it a cost-effective and noninvasive method for predicting fluid responsiveness in patients.
In a prospective observational study conducted in a 10-bed intensive care unit, fifty adult patients with acute circulatory failure were enrolled. Each patient received a standardized 500-mL intravenous fluid bolus. Fluid responsiveness was determined using transthoracic echocardiography, with PPI recorded before and after the bolus to calculate the relative change (ΔPPI).
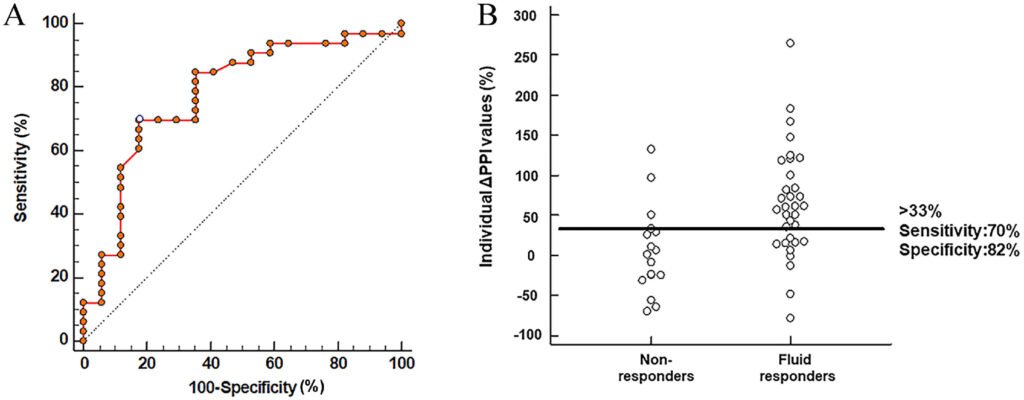
Results showed that a 33% increase in PPI correctly identified responders with 70% sensitivity and 82% specificity. While the overall diagnostic accuracy was moderate, with an area under the ROC curve of 0.78, a “gray zone” of inconclusive values highlighted the importance of interpreting ΔPPI alongside other clinical signs.
Although ΔPPI did not align perfectly with echocardiographic changes, there was a 70% agreement between the two measures, indicating that PPI captures real trends in stroke volume changes. The accessibility and simplicity of PPI, derived from standard pulse oximeters, make it an attractive option for hospitals with limited resources or during emergency situations.
Dr. Younes Aissaoui, the corresponding author of the study, emphasized the significance of ΔPPI as a pragmatic tool for fluid management, especially in settings where advanced monitoring is unavailable. Larger multicenter trials are needed to confirm these results and refine thresholds for clinical use, with a focus on complementing, rather than replacing, clinical judgment and echocardiography.
As research continues to explore the potential of PPI in guiding resuscitation decisions in intensive care, the integration of technological advancements and other hemodynamic indicators may further enhance its diagnostic performance and clinical utility. This study contributes to a global effort to develop practical tools for critical care that can be utilized worldwide, irrespective of economic resources or technological sophistication.