Keloids are a type of raised, overgrown scars that can develop after skin injuries or surgery, often extending beyond the original wound boundaries. These scars not only pose a cosmetic concern but also lead to distressing symptoms such as chronic pain, itching, and restricted movement for many individuals. Despite the availability of various treatment options like surgical removal, steroid injections, and radiation, keloids remain challenging to manage, with recurrence rates as high as 30%.
The exact reason behind the uncontrollable growth of keloids, unlike hypertrophic scars, has remained a mystery even after decades of research. It is believed that the overproduction of collagen by fibroblasts, cells responsible for producing connective tissue components, plays a role in keloid formation. Additionally, repeated mechanical tension on the skin is thought to contribute to this condition. However, the specific cellular and molecular mechanisms driving this abnormal scarring process are not fully understood.
A recent study published in The Journal of Pathology on September 1, 2025, sheds new light on the underlying mechanisms of keloid formation. Led by Professor Yuzuru Ikehara from Chiba University, Japan, the research team, including Dr. Shinsuke Akita, Dr. Sanae Ikehara, Prof. Kiyoshi Hirahara, and Prof. Nobuyuki Mitsukawa, conducted a comprehensive analysis of keloid tissues to identify the unique drivers of keloid formation and recurrence.
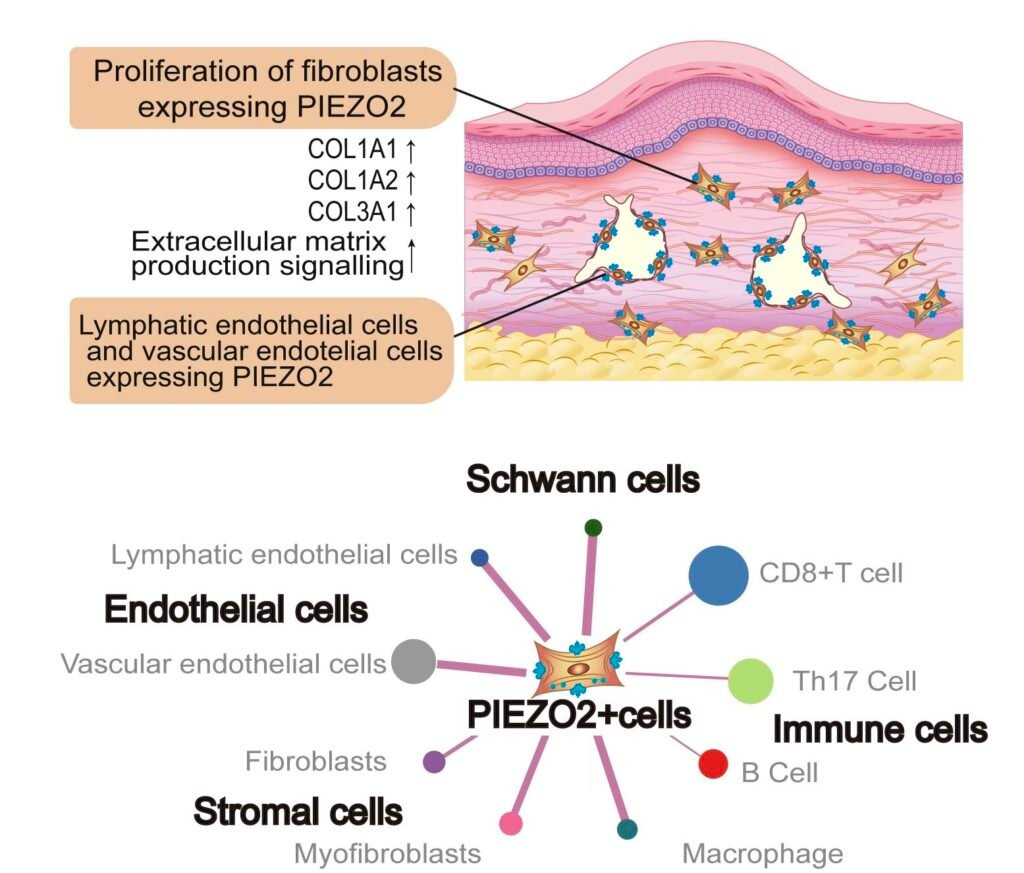
By comparing keloid tissues with those from lymphedema, a condition characterized by fibrous overgrowth but not primarily driven by mechanical tension, the researchers aimed to pinpoint the specific alterations in keloid fibroblasts. Through advanced techniques like global gene expression analysis and single-cell RNA sequencing, the team identified a key player in keloid pathology—PIEZO2, a mechanosensitive ion channel.
The study revealed that keloid tissues exhibited significantly higher levels of PIEZO2 compared to lymphedema tissues. Moreover, keloids with a history of recurrence showed even higher expression of PIEZO2. Further analysis identified a subpopulation of fibroblasts expressing high levels of PIEZO2, termed FB
These PIEZO2-expressing fibroblasts were found clustered around blood and lymphatic vessels in keloids, particularly in areas of active growth. This discovery opens up new possibilities for the diagnosis and treatment of keloids, highlighting the importance of tension-sensing cells in the pathogenesis of this condition.
Moving forward, the identification of PIEZO2-expressing fibroblasts could lead to the development of targeted therapies, such as PIEZO2 inhibitors, to alleviate keloid-related symptoms like pain and itching. By understanding the unique cellular and molecular mechanisms driving keloid formation, researchers aim to improve patient outcomes and enhance the quality of life for individuals affected by this challenging condition.