The Challenges of Accessing Mental Health Care After Release from Incarceration
Valentino Valdez’s story sheds light on the struggles faced by many individuals after being released from prison or other correctional facilities. Despite being provided with basic necessities like a birth certificate and Social Security card, Valdez found himself lacking crucial resources like health insurance, mental health medications, and access to a doctor upon his release from a Texas prison in 2019 at the age of 21. This lack of support led him to a mental health crisis that resulted in hospitalization three years later.
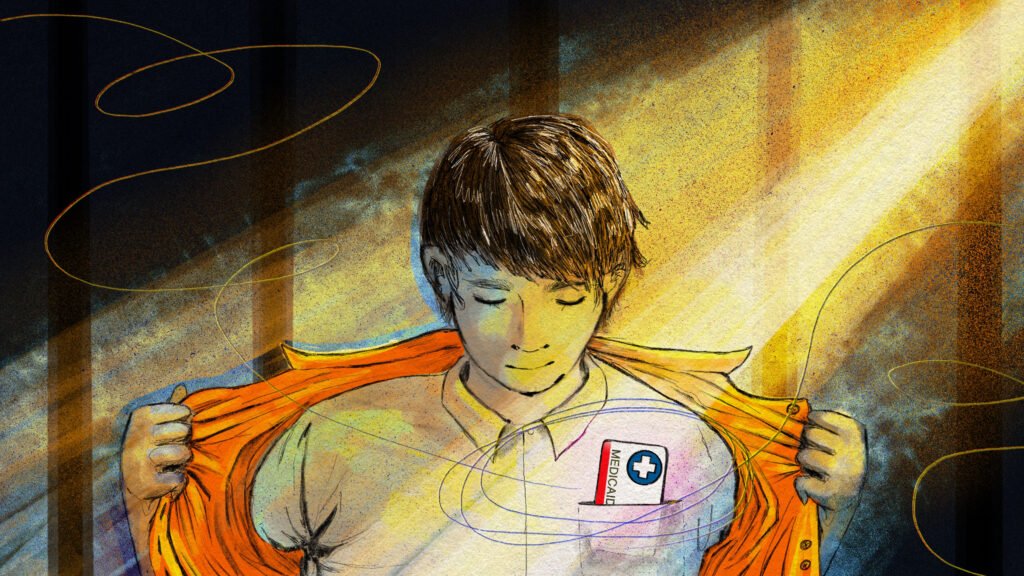
Valdez’s experience highlights a common issue faced by individuals reentering society after incarceration. Many are left to navigate the complex healthcare system on their own, often leading to adverse outcomes such as relapse, reoffending, or even death. Recognizing the need for better support for this population, a new federal law was enacted in 2022 to connect incarcerated children and young adults who are eligible for Medicaid or the Children’s Health Insurance Program (CHIP) to healthcare services before their release.
The law requires all states to provide medical and dental screenings to Medicaid- and CHIP-eligible youths 30 days before or immediately after their release from a correctional facility. Additionally, youths must receive case management services for 30 days post-release. This initiative aims to prevent health crises, improve reintegration into society, and reduce recidivism rates among this vulnerable population.
While the new law holds promise for improving the health outcomes of individuals leaving incarceration, its implementation poses significant challenges. Correctional facilities and state health agencies must establish systems to identify eligible youths, find healthcare providers who accept Medicaid, bill the federal government, and share records and data. This process requires coordination and collaboration among multiple stakeholders, and it may take time for facilities to fully comply with the new requirements.
Despite the obstacles, advocates believe that the law represents a crucial step towards addressing the neglected healthcare needs of individuals transitioning out of incarceration. By ensuring access to essential healthcare services, states can potentially reduce healthcare costs, emergency care visits, and recidivism rates. However, the success of the law will depend on the willingness of states to prioritize and invest in the health and well-being of this underserved population.
Valdez’s journey serves as a reminder of the profound impact that access to mental health care can have on individuals reentering society after incarceration. By providing comprehensive support and resources to those in need, we can help break the cycle of trauma, incarceration, and poor health outcomes, creating a more equitable and compassionate system for all.