Semen analysis has long been used as a tool to assess male fertility, but researchers at the University of Adelaide are exploring its potential to promote healthier lifestyles. Dr. Hannah Lyons and Dr. Nicole McPherson from the University’s School of Biomedicine and Robinson Research Institute believe that semen analysis could be a key indicator of long-term health risks for men.
The process of spermatogenesis, or the development of mature sperm cells, is a delicate one that can be influenced by various factors. A traditional semen analysis typically measures physical volume, pH, sperm concentration, movement, form, and viability of sperm samples. While not a definitive measure of fertility, this analysis provides valuable insights into reproductive health, which is an essential component of overall well-being.
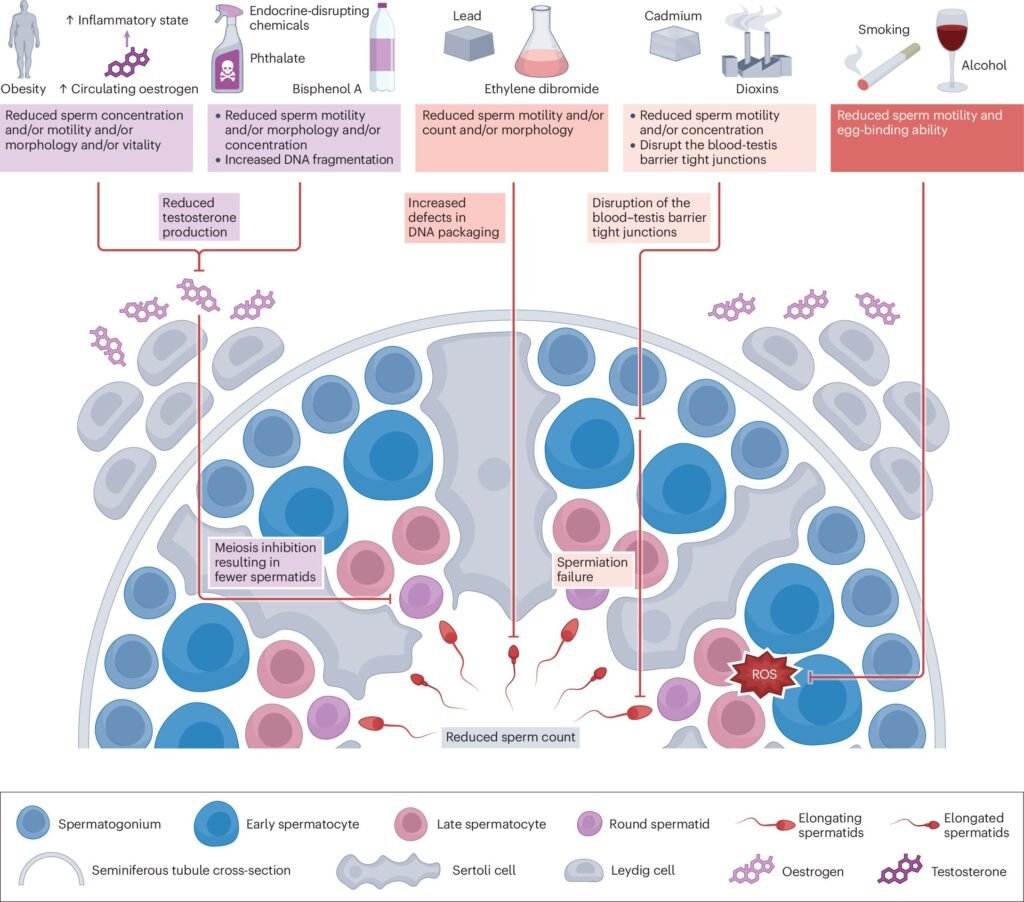
In a recent review published in the journal Nature Reviews Urology, the researchers delve into the complexities of male fertility, the impact of lifestyle and environmental factors on semen quality, and the potential for using semen analysis to motivate lifestyle changes and reduce chronic disease risk in men. They highlight that male fertility is heavily influenced by environmental, lifestyle, and medical factors, with evidence suggesting that interventions like nutritional supplementation and lifestyle changes can improve semen quality and fertility potential.
Factors such as obesity, recreational drug use, high-intensity exercise, smoking, and alcohol consumption can all have a significant impact on sperm quality. However, Dr. McPherson emphasizes that making positive lifestyle changes can lead to rapid and meaningful improvements in reproductive health. She also stresses the importance of delivering abnormal semen analysis results with empathy and respect, as men may perceive such news as a blow to their masculinity.
By incorporating male fertility assessments into broader health evaluations, the researchers believe that the stigma around male infertility can be reduced, and awareness about the importance of reproductive health in overall well-being can be increased. Men who are motivated to start a family are likely to respond well to preconception care advice and lifestyle interventions aimed at improving fertility and general health.
The study by Dr. Lyons and Dr. McPherson underscores the potential of semen analysis as a valuable tool for predicting broader health concerns in men. By leveraging this information, healthcare providers can offer targeted interventions and support to improve not only fertility but also overall health outcomes for men. This holistic approach to male health could change the narrative around reproductive health and encourage men to take proactive steps towards healthier living.
For more information, you can access the original study titled “Unlocking the power of semen analysis in primary health care — a path to men’s health and lifestyle transformation” published in Nature Reviews Urology.