Thymic epithelial tumors are a rare group of malignancies that originate in the thymus gland, which includes thymoma and thymic carcinoma. Thymic carcinoma is the more aggressive subtype, known for its high invasiveness, metastatic potential, and poor prognosis.
Despite its rarity, with an incidence of just 0.15 cases per 100,000 person-years, thymic carcinoma poses significant challenges for treatment development. While platinum-based chemotherapy is the current standard of care, its effectiveness is limited. Immune checkpoint inhibitors have shown promise in pretreated cases, but there is a critical unmet need for durable and effective systemic therapies for chemotherapy-naïve patients.
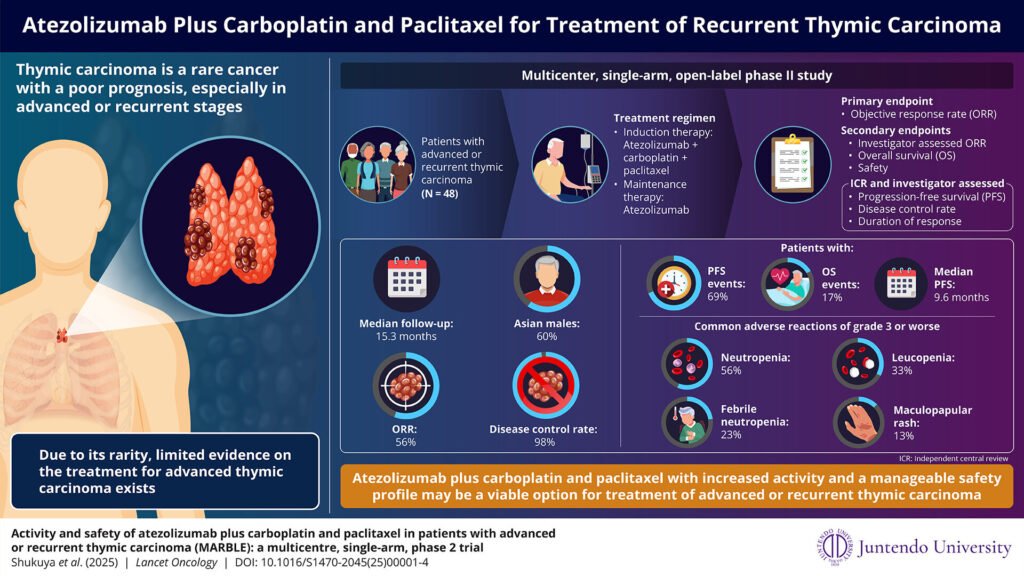
To address this issue, a team of researchers led by Associate Professor Takehito Shukuya from the Department of Respiratory Medicine at Juntendo University, Japan, conducted the MARBLE study. This study aimed to evaluate the combination of atezolizumab, an immune checkpoint inhibitor, with carboplatin and paclitaxel in patients with advanced or recurrent thymic carcinoma.
The results of the MARBLE study, published in The Lancet Oncology, demonstrated promising outcomes. With a median follow-up of 15.3 months, the combination therapy achieved an objective response rate of 56% and a median progression-free survival of 9.6 months, surpassing historical chemotherapy outcomes. The disease control rate was 98%, with 56% of patients showing partial responses and 42% maintaining stable disease.
The safety profile of the treatment was consistent with known effects, with no new safety concerns or treatment-related deaths reported. Adverse events were manageable, with common severe events including neutropenia, leukopenia, maculopapular rash, and febrile neutropenia. Patients with higher programmed cell death ligand 1 expression exhibited longer progression-free survival, indicating its potential as a predictive biomarker for treatment response.
Overall, the MARBLE study presents a promising therapeutic option for advanced thymic carcinoma by combining immune checkpoint inhibitors with platinum-based chemotherapy. The results suggest that this combination regimen could become a new standard of care for this rare and challenging disease, offering hope for improved outcomes and long-term disease control for patients.
In conclusion, the MARBLE study highlights the potential of atezolizumab combined with carboplatin and paclitaxel as an effective and well-tolerated treatment option for advanced thymic carcinoma. This innovative approach addresses the therapeutic gap in this disease, providing optimism for better outcomes and extended disease control in affected patients.