This past week served as a stark reminder of the challenges in finding effective treatments for Alzheimer’s disease. Two major pharmaceutical companies, Johnson & Johnson and Novo Nordisk, both experienced setbacks in their respective Phase 2 and Phase 3 clinical trials, despite investing billions of dollars and years of research.
A Double Dose Of Disappointment
Johnson & Johnson’s experimental anti-tau antibody, posdinemab, which was once projected to generate over $5 billion in annual sales, failed to slow cognitive decline in early-stage Alzheimer’s patients. In a similar vein, Novo Nordisk’s semaglutide, a drug known for its success in treating obesity, also failed to meet its primary endpoints in trials for early Alzheimer’s disease, leading to a drop in the company’s stock value.
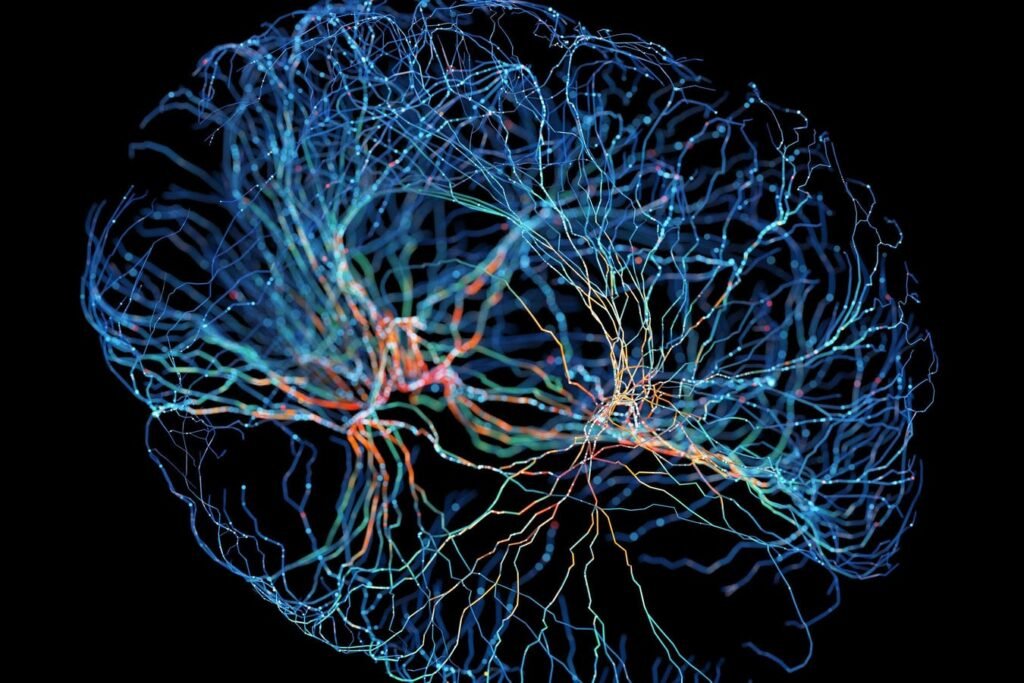
These recent failures highlight the complexity of Alzheimer’s disease, which proves to be resistant to single-target interventions, whether they are rooted in neurobiology or metabolism.
The Rise And Fall Of Anti-Tau Therapy
For over a decade, the tau hypothesis has been considered a promising approach in Alzheimer’s research, focusing on targeting tau tangles that are believed to drive neuronal dysfunction and cognitive decline. However, despite the theoretical potential of anti-tau antibodies to block the spread of abnormal tau in the brain, clinical trials have consistently yielded disappointing results.
Multiple drug candidates, including Roche’s semorinemab and UCB’s bepranemab, have failed in trials, underscoring the challenges in developing effective anti-tau therapies for Alzheimer’s disease.
Even Johnson & Johnson’s posdinemab, which targeted phosphorylated tau, failed to show significant benefits in slowing cognitive decline in Alzheimer’s patients, leading to the discontinuation of its development.
Novo’s GLP-1 Alzheimer’s Bet Falls Flat
In contrast to the neurobiology approach, Novo Nordisk’s disappointment with semaglutide reflects the difficulties of applying metabolic medicine to Alzheimer’s disease. Despite promising preclinical data suggesting the potential benefits of GLP-1 receptor activation in reducing amyloid and tau accumulation, the EVOKE and EVOKE+ trials showed no improvement in disease progression in early Alzheimer’s patients.
The setbacks in both neurobiological and metabolic approaches highlight the complexity of Alzheimer’s disease and the challenges in finding effective treatments that can address its multifactorial nature.
Why GLP-1 And Metformin Looked Bright
The enthusiasm for GLP-1 and metformin in Alzheimer’s research was based on the connection between Alzheimer’s and metabolic dysfunction, known as “type 3 diabetes.” Drugs like liraglutide and metformin showed early promise in slowing cognitive decline and reducing brain atrophy in smaller studies.
However, the recent clinical trial failures suggest that the benefits of these drugs may be more pronounced in early or preclinical stages of the disease, rather than in later stages when symptoms are already present.
Where The Field Goes
Despite these setbacks, the Alzheimer’s research pipeline remains active, with ongoing trials of new tau-targeting antibodies like BMS-986446 from Bristol Myers Squibb and antisense tau approaches from Biogen. Additionally, metformin precision-medicine initiatives aim to identify patient subtypes that may benefit from metabolic therapies.
While progress in Alzheimer’s research may seem slow, each setback serves as a valuable data point that brings researchers closer to understanding the complex mechanisms underlying the disease and, potentially, finding effective treatments in the future.