Your gut-brain axis, hunger hormones, and environment collaborate to determine your eating habits and satiety cues.
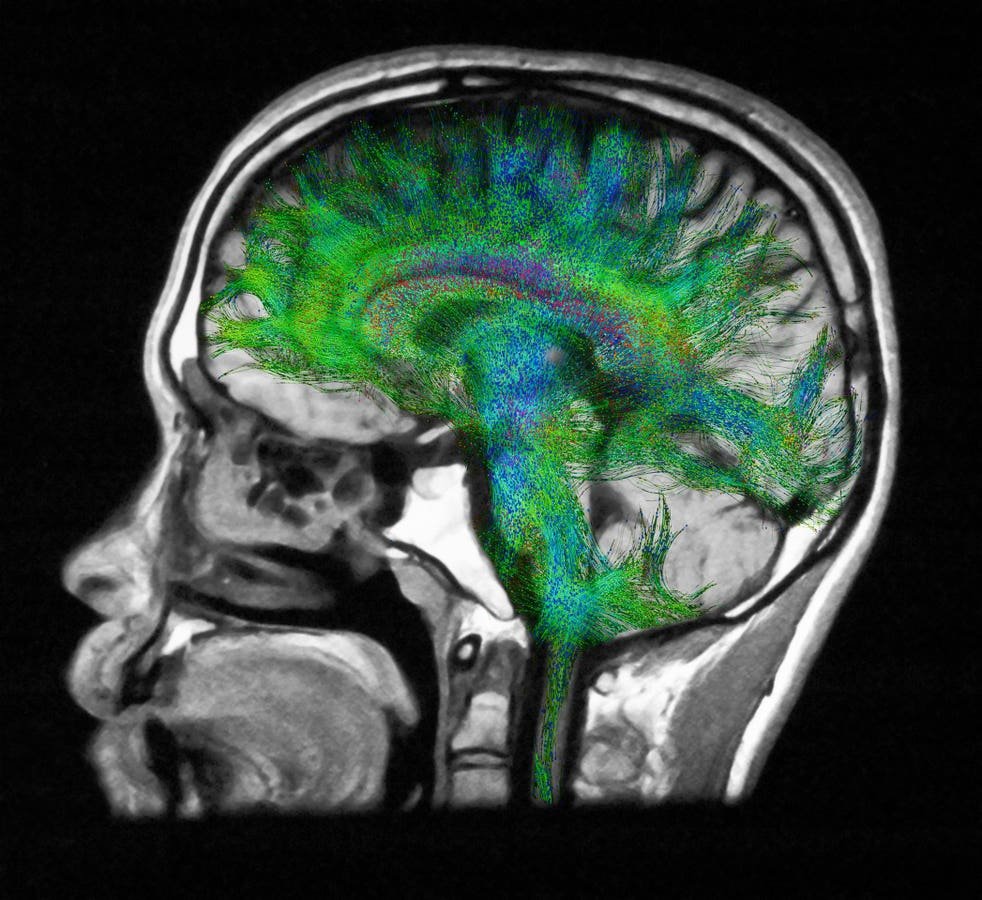
Diffusion MRI of the brain.
getty
Questions about hunger and fullness are common in my practice. Many individuals try to manage their appetite using sheer willpower without realizing the complex biological systems influencing their hunger and satisfaction levels.
Each time you eat or decide not to, you are engaging with a sophisticated network of communication between your gut, brain, hormones, and surroundings. This intricate system dictates your hunger pangs, food cravings, and feelings of fullness. Understanding the workings of these short-term appetite signals is crucial to comprehending how your body regulates hunger, fullness, and weight.
This article kicks off a five-part Forbes Health series delving into the biological mechanisms controlling hunger and fullness, their impact on long-term weight management, the reasons for their occasional malfunction, and how modern treatments can target them.
Key Concepts in Appetite Control
Before delving into the physiology, it’s beneficial to clarify a few fundamental concepts. Appetite control encompasses two interconnected yet distinct processes. Satiation comprises the signals prompting you to cease eating during a meal. Satiety denotes the sensation of fullness and decreased appetite post-meal, delaying the return of hunger.
Another vital differentiation lies between homeostatic hunger, indicative of genuine energy requirements, and hedonic hunger, driven by the brain’s reward mechanisms and leading to eating for pleasure rather than necessity.
These concepts frame the interaction among the gut, brain, and hormones in managing appetite both in real-time and over the long haul.
How the Gut-Brain Axis Controls Appetite
Central to this process is the gut-brain axis, establishing a bidirectional communication pathway linking the digestive system to the brain through hormonal signaling, nerve pathways, and metabolic feedback. The hypothalamus, situated deep within the brain, integrates these incoming signals and determines whether to stimulate or suppress appetite.
Two pivotal neuronal clusters lie at the crux of this regulation:
- NPY/AgRP neurons trigger hunger, urging you to seek sustenance.
- POMC/CART neurons foster satiety and diminish intake.
These neurons consistently receive input from the gut and other organs, fine-tuning appetite moment by moment. It’s a sophisticated, dynamic system rather than a simple on-off switch.
Hunger Hormones That Influence Eating Patterns
Your gut functions as an endocrine organ, secreting a sequence of hormones in response to fasting and feeding. These hunger and satiety hormones travel through the bloodstream, directly communicating with the brain. Here are some crucial players:
- Ghrelin: Originating in the stomach, ghrelin, dubbed the hunger hormone, surges before meals and diminishes post-eating. Ghrelin not only induces hunger but also triggers reward pathways, heightening the allure of food.
- Cholecystokinin (CCK): Released by cells in the upper small intestine upon fat and protein ingestion, CCK furnishes one of the earliest signals indicating satiety. It decelerates gastric emptying and prompts vagal nerve signals promoting fullness.
- GLP-1 (Glucagon-like peptide 1) and PYY (Peptide YY): Released further down the digestive tract, predominantly from the ileum and colon as nutrients progress, these hormones sustain satiety, delay gastric emptying, and suppress appetite for hours post-meal. GLP-1 has garnered significant attention as the target of medications like semaglutide and tirzepatide.
- GIP (Gastric inhibitory polypeptide): Another incretin hormone playing a complementary role by boosting insulin secretion and modulating appetite. Novel combination therapies target both GLP-1 and GIP for enhanced efficacy.
- Bile acids: Beyond aiding digestion, bile acids activate receptors in the gut like TGR5 and FXR, which can impact GLP-1 secretion and energy metabolism, introducing an additional layer to appetite control.
The timing and equilibrium of these hormonal signals play a crucial role in determining your pre-meal hunger and post-meal satisfaction.
The Role of the Vagus Nerve in Appetite and Satiety
The vagus nerve serves as the primary rapid communication conduit between the gut and the brain. It relays real-time details on stomach and bowel mechanical stretch, as well as the chemical milieu, aiding the brain in initiating satiation. When food enters the stomach, stretch receptors activate, dispatching instantaneous neural signals contributing to the decision to cease eating.
Specialized sensory cells in the gut lining also respond to nutrients, releasing neurotransmitters and hormones that add additional layers of signaling. These hormonal effects reach the brain more slowly through the bloodstream, playing a greater role in satiety, the enduring sensation of fullness post-meal. Consuming slowly allows the rapid vagal signals and the slower hormonal pathways to synergize, enhancing the body’s capacity to sense and respond to food intake.
How the Gut Microbiome Affects Hunger and Satiety
The myriad bacteria inhabiting your gut wield a pivotal influence on appetite regulation and digestion. They generate short-chain fatty acids like acetate, propionate, and butyrate upon fermenting dietary fiber. These short-chain fatty acids spur the release of PYY and GLP-1, fortify gut barrier integrity, and may even communicate directly with the vagus nerve.
Specific bacterial profiles are linked to heightened satiety hormone production, while others might spur overeating. Though this realm is still evolving, it’s increasingly evident that the microbiome isn’t merely a passive bystander. It’s an active metabolic organ shaping your hunger or fullness.
How Sleep, Stress, and Circadian Rhythms Impact Appetite and Fullness
Woman working late at home
getty
Appetite signaling doesn’t operate in a vacuum. Everyday factors like sleep, stress, and light exposure can swiftly disrupt or amplify the same hormonal pathways regulating hunger and satisfaction. Research over the past couple of decades has shown that these factors can alter levels of leptin, ghrelin, and cortisol, and affect how responsive the brain remains to these signals.
Sleep deprivation
Mere nights of inadequate sleep can tangibly alter appetite hormones. Seminal research from the University of Chicago published in Annals of Internal Medicine in 2004 revealed that restricting sleep to four hours per night for just two days reduced circulating leptin, the hormone signaling fullness and regulating body weight, and elevated ghrelin, which spurs hunger. A sizable population study published in PLOS Medicine the same year corroborated these findings, associating shorter sleep duration with heightened ghrelin, lower leptin, and ultimately a higher body mass index. Subsequent research published in The Journal of Clinical Endocrinology & Metabolism in 2012 demonstrated that sleep loss also heightens brain reward responses to high-calorie foods, suggesting heightened brain reactivity to food cues when fatigued. This confluence of reduced leptin signaling, increased ghrelin, and heightened reward sensitivity creates an ideal environment for overeating.
Although leptin primarily governs longer-term energy balance and body weight, these studies elucidate how short-term alterations in leptin can influence appetite and fullness during sleep deprivation or stress, linking it to both immediate and protracted intake regulation.
Stress and cortisol
Amid acute and chronic stress, the adrenal glands discharge cortisol, a hormone mobilizing energy while also impacting appetite and food selection. Research from the University of California, San Francisco, published in Psychoneuroendocrinology in 2001 found that heightened cortisol raises appetite and inclines individuals toward energy-dense comfort foods, particularly those rich in sugar and fat. Prolonged elevated cortisol levels can compromise leptin signaling, impeding the brain’s ability to recognize satiety.
Circadian rhythm misalignment
Timing is as critical as quantity. Research from Harvard Medical School published in Proceedings of the National Academy of Sciences in 2009 demonstrated that circadian misalignment, like during shift work or frequent time zone changes, disrupts normal leptin and ghrelin cycles. Leptin levels dip and ghrelin spikes during times when the body should be at rest, provoking nocturnal hunger and reduced satiety post-meal. These hormonal shifts occur even with adequate total sleep duration, underscoring how sensitive appetite regulation is to light exposure and meal timing.
Collectively, these studies reveal that sleep, stress, and circadian rhythm serve as potent short-term appetite regulators. Each can diminish leptin or blunt leptin receptivity, heighten ghrelin, and modify cortisol balance, fostering increased hunger and intensified cravings. In practical terms, feeling fatigued, stressed, or off-kilter doesn’t merely make eating more enticing. It alters the underlying biology dictating when and how much you desire to eat.
Hedonic Hunger vs Homeostatic Hunger
Dessert temptation after dinner
getty
Not all hunger stems from physiological need. Homeostatic hunger emanates from genuine energy requirements and gut-brain signaling, albeit this can veer off course as we’ll explore in subsequent segments. Hedonic hunger, conversely, stems from the brain’s reward circuits, typically triggered by hyper-palatable foods blending sugar, fat, and salt in ways overriding natural satiety mechanisms.
Hedonic hunger is chiefly governed by dopamine, the neurotransmitter reinforcing behaviors linked to pleasure and reward. When indulging in highly palatable foods, dopamine floods brain regions like the nucleus accumbens, generating feelings of contentment and imprinting the brain to repeat the behavior. Over time, cues like sight or aroma can trigger dopamine release even before eating commences, heightening cravings. Research from the National Institute on Drug Abuse published in Nature Neuroscience in 2011 revealed that these dopamine responses can manifest even in individuals not physiologically hungry, elucidating why food cravings often persist despite feeling full.
This differentiation is pivotal. Craving dessert after a substantial dinner may not stem from caloric necessity but from continued activation of the brain’s reward system. Modern food environments exploit this biological loophole persistently, keeping appetite and cravings incessantly stimulated.
Hunger Hormones vs Long-Term Weight Regulation
These short-term appetite mechanisms expound why hunger strikes, why satiety takes time to register, and why sleep and stress can derail your eating patterns. However, they don’t encapsulate the entirety of the narrative behind why individuals gain or shed weight over extended periods.
Your body also houses a long-term thermostat regulating weight via hormones like leptin and insulin, modulating both appetite and energy expenditure to sustain a body weight set point. This system, its functionality, and why it frequently drifts upward are the focal points of the subsequent article in this series.
The Takeaway
Hunger and fullness aren’t voluntary occurrences. They epitomize coordinated communication among the gut, brain, and hormones operating largely beyond conscious influence. Grasping the mechanics of these pathways clarifies why hunger can seem capricious and why strategies honoring the body’s internal cues prove more efficacious than those opposing them.